Optimize your billing workflow and get paid faster!
Billing is the backbone of your organization. You want, and need, to be reimbursed for the services your team delivers as quickly as possible. When your billing system is integrated with your service delivery platform, reimbursement timeframes get shorter. However, when Medicaid claims, billing, and service delivery are done on the same IDD software platform, your revenue cycle really accelerates. Our comprehensive billing software for IDD agencies is an eVero difference!
ACCELERATE™, the comprehensive billing, payment, and revenue management module of the eVero platform, gives you full control of your Medicaid, State-Paid, Self-Paid, and MCO billing right from the eVero platform. Automated workflows collect service details from our platform database and efficiently generate, validate, submit, and track electronic claims, so you get paid as fast as possible. Customizable dashboard views also let you track actual revenue and potential receivables, empowering you with real-time insight into your cash flow. And with no clearinghouse or third-party billing provider fees, your processing costs are reduced as well.

Submit Claims Faster
Designed with your ease of use in mind, all required service data is already captured by and stored on the eVero platform, so you can create, approve, and submit claims the same day that the service is delivered. What’s more? You can even do batch submissions for faster and more efficient service.
Realize Revenue Sooner
Our streamlined claims process eliminates delays associated with obtaining service data from outside EHR systems or reviewing and resubmitting denied claims, accelerating the payment cycle.
Ensure Claim Accuracy
Checks and balances are built in for greater accuracy. For example, data validation tools, combined with daily Medicaid eligibility checks, verify that each claim is coded properly and error-free before being submitted. You can feel confident when you submit claims using ACCELERATE™.

Gain insight into your Entire Revenue Cycle
Have clarity and insight into actual and potential cash flow with customizable dashboards – which include payments, current accounts receivable, and projected receivables, so you always know where you stand.
Preview Projected Cash Flow
Since eVero is the system of record for service delivery, ACCELERATE™ can provide a preview of future revenue based on services delivered but not yet billed.
Increase Operational Efficiency
Stay ahead with automated alerts. The system provides notifications on time-sensitive items, such as the Medicaid 90-day submission deadline or ePaces recertification so you don’t risk lapsing or expiring.
Be Audit-Ready
Always be prepared! Since all submitted claims are linked to the actual service records stored on our platform, providing easy access to support documentation can simplify the audit process.

Reduce Costs
Every claim submitted with any error can cost you time and money. Waiting on third-party billing providers or clearinghouses is an unnecessary dependency that can delay you, not to mention it’s an additional business cost. Put more back into your business with ACCELERATE™–which removes the need for 3rd parties and seamlessly reconciles services and claims, all helping you to reduce costs.
Other ACCELERATE™ highlights:
- Cloud-based; automatically updated to meet regulatory and compliance changes
- Easily integrates with third-party Accounting, General Ledger, and EHR systems
- Conducts daily Intake Claim and Medicaid Eligibility verification checks
- Standard and customized report options, all exportable
- Unparalleled support, from onboarding to Help Desk (email, phone, chat)
- 100% HIPAA EDI Compliant

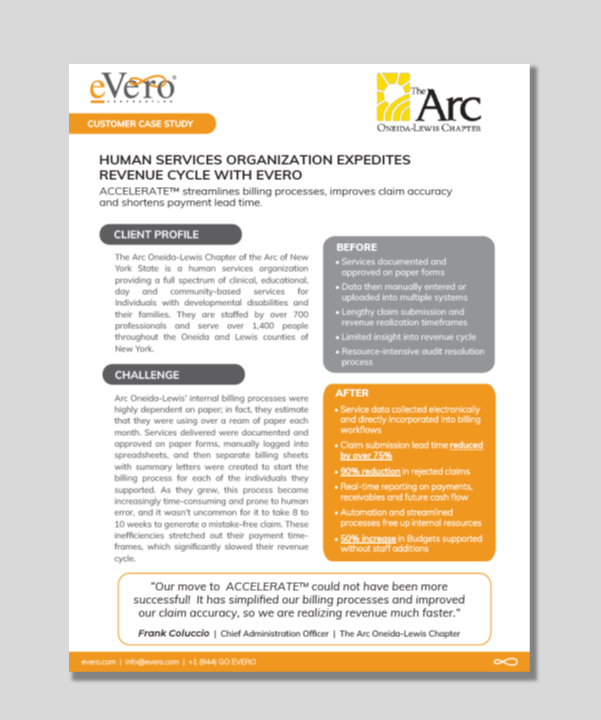
Case Study
ACCELERATE™ helps I/DD Agency simplify billing, improve claim accuracy and realize revenue faster.
Arc Oneida-Lewis’ Medicaid, State-Pay, Self-Paid, and MCO billing processes were highly dependent on paper forms, spreadsheets, and manual processes. As it grew, this became increasingly time-consuming and prone to human error, and it wasn’t uncommon for it to take 8 to 10 weeks to generate a mistake-free claim.
This growing agancy turned to eVero’s ACCELERATE™ to streamline its billing operations and speed up its revenue cycle.
Read the full Case Study to learn how eVero helped them reach new levels of efficiency and transparency while shortening revenue realization timeframes by over 50%!
Are you ready to optimize your billing and maximize your revenues?
Please complete the form below and we’ll be in touch!











